Lyme Disease Symptoms & Treatment
Lyme disease is one of the most common tick-transmitted diseases in the world but only causes symptoms in 5-10% of affected dogs. It is caused by a spirochete (bacteria) species of the Borrelia burgdorferi group. When infection leads to disease in dogs, the dominant clinical feature is recurrent lameness due to inflammation of the joints. There may also be a lack of appetite and depression. More serious complications include damage to the kidneys, and rarely, heart or nervous system disease.
Kidney disease appears to be more prevalent in Labrador retrievers, golden retrievers, Shetland sheepdogs, and Bernese Mountain dogs. Experimentally, young dogs appear to be more susceptible to Lyme disease than older dogs. Transmission of the disease has been reported in dogs throughout the United States and Europe, but is most prevalent in the upper Midwestern states, the Atlantic seaboard, and the Pacific coastal states.
SYMPTOMS AND TYPES
Many dogs who develop Lyme disease have recurrent lameness due to inflammation of the joints. Sometimes the lameness lasts for only three to four days but recurs days to weeks later, either in the same leg or in other legs. This is known as “shifting-leg lameness.” One or more joints may be swollen, warm, and painful.
Some dogs may also develop kidney problems. Lyme disease sometimes leads to glomerulonephritis – inflammation and accompanying dysfunction of the kidney's glomeruli (essentially, a blood filter). Eventually, kidney failure may set in as the dog begins to exhibit such signs as vomiting, diarrhea, lack of appetite, weight loss, increased urination and thirst, and abnormal fluid buildups.
Other symptoms associated with Lyme disease include:
- Stiff walk with an arched back
- Sensitivity to touch
- Difficulty breathing
- Fever, lack of appetite, and depression
- Superficial lymph nodes close to the site of the infecting tick bite may be swollen
- Heart abnormalities are reported, but rare
- Nervous system complications (rare)
CAUSES
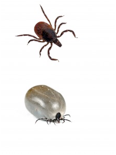
Borrelia burgdorferi, which is the bacteria responsible for Lyme disease, is transmitted by slow-feeding, hard-shelled deer ticks (Ixodes spp.).Infection typically occurs after the Borrelia-carrying tick has been attached to the dog for at 2-3 days.

If you live in a Lyme disease endemic area such as the Northeast and upper Midwest and your dog is the outdoorsy type who picks up ticks on his adventures, you can use homeopathy to good effect in protecting him against Lyme disease.
When you find a tick on your dog, the first thing to do is remove the tick as soon as possible.
Save the tick by placing it in a covered jar with either 180 proof vodka, grain alcohol or brandy and label it with the date, on whom it was found and where on the body. In the unlikely event that all else fails, the tick can be made into a homeopathic remedy. This is known as isopathy, which works under principles similar to homeopathy.
But for now, just keep the tick in a jar.
Then follow whichever steps below are appropriate for your dog’s situation, depending on how long ago the bite occurred and whether he is displaying any symptoms of Lyme disease.
For prevention after a recent bite, this has been found to be highly effective for bites that are rather recent – say within a few weeks.
Remedy: Ledum palustre 200CYourPetsAndLymeDisease.pdf
Ledum is the foremost remedy for any kind of animal bite.
- Give the first dose of this remedy at the time you remove the tick.
- Continue dosing with Ledum every 3 hours for the first day
- Then, dose twice daily for a week
- After the first week, dose twice weekly for a month
- Then once per week for another month
This is probably overkill, but worth the extra effort to be certain.
Remedy: Aurum arsenicum 200C
Aurum arsenicum is a capital choice for when a poisonous infection arises, and this is one of those times.
- Dose twice daily for one week
- After the first week, dose twice weekly for a month
- Then once per week for another month
DIAGNOSIS
You will need to give a thorough history of your dog's health, including a background of symptoms and possible incidents that might have precipitated them. The history you provide may give your veterinarian clues as to which organs are being affected. Your veterinarian may run some combination of blood chemistry tests, a complete blood cell count, a urinalysis, fecal examinations, X-rays, and tests specific to diagnosing Lyme disease (e.g., serology). Fluid from the affected joints may also be drawn for analysis.
In older cases of Lyme, the most common symptoms in dogs are arthritis or painful joints and lameness; other symptoms may include fever, lack of appetite, depression or lethargy. Dogs do not exhibit the classic “bulls eye” rash that occurs in humans. Symptoms can occur two to five months after exposure. If your dog shows these symptoms, it’s best to consult an experienced homeopathic vet who can prescribe the correct remedy for his symptoms, along with the above procedures.
There are many causes for arthritis, and your veterinarian will focus on differentiating arthritis initiated by Lyme disease from other inflammatory arthritic disorders, such as trauma, degenerative joint disease, or osteochondrosis dissecans (a condition found in large, fast growing breeds of puppies). Immune-mediated diseases will also be considered as a possible cause of the symptoms. An X-ray of the painful joints will allow your doctor to examine the bones for abnormalities.
TREATMENT
If the diagnosis is Lyme disease, your dog will be treated as an outpatient unless their condition is unstable (e.g., severe kidney disease). Doxycycline is the most common antibiotic that is prescribed for Lyme disease, but others are also available and effective. The recommended treatment length is usually four weeks, but longer courses may be necessary in some cases. Your veterinarian may also prescribe an anti-inflammatory (pain reliever) if your dog is especially uncomfortable.
Unfortunately, antibiotic treatment does not always completely eliminate infection with Borrelia burgdorferi bacteria. Symptoms may resolve but then return at a later date, and the development of kidney disease in the future is always a worry.
LIVING AND MANAGEMENT
Improvement in sudden (acute) inflammation of the joints caused by Borrelia should be seen within three to five days of antibiotic treatment. If there is no improvement within three to five days, your veterinarian will want to reevaluate your dog.
It appears that doxycycline, tetracycline and amoxicillin seem to be the best antibiotics against Lyme disease. I suggest staying on antibiotics for a minimum of a month, sometimes even longer. I have seen dogs that were only on antibiotics for two weeks and then it comes back with a vengeance and does not respond as well afterwards. A holistic integrative approach would also include using probiotics such as acidophilus to keep the healthy bacteria alive in your pet’s gastrointestinal tract. In addition, it has been found that the organism can actually further suppress the immune system. So I usually recommend nutritional and herbal support to boost the immune system as well. This would include a specifically prepared form of a western herb, prima una de gato, specific Chinese herbal formula and medicinal mushrooms. Sometimes I see chronic Lyme disease in a dog or cat and I will also use acupuncture to boost the immune system and relieve the pain and inflammation. Though homeopathy still appears to be controversial, in my experience I have found certain homeopathic remedies that may sometimes be helpful. The most successful of these include homeopathic Ledum and a Lyme nosode. Lyme nosode is a homeopathic remedy that is made from the killed organism, diluted, successed and potentized to the point that nothing of the original organism remains. For appropriate dosages of these remedies, you should contact a homeopathic veterinarian.
PREVENTION
If possible, avoid allowing your dog to roam in tick-infested environments where Lyme disease is common. Check your dog’s coat and skin daily and remove ticks by hand. Your veterinarian can also recommend a variety of sprays, collars, and spot-on topical products that kill and repel ticks. Such products should be used under a veterinarian's supervision and according to the label's directions. Lyme vaccines are available, but their use is somewhat controversial. Talk to your veterinarian to see if Lyme vaccination is right for your dog.
The best prevention still is checking your dog carefully and removing any ticks at least once a day. Collars do not seem to work that well, though newer ones seem a bit more effective. Some of the topical insecticides do seem to work well, but then one has to weigh the potential toxic effects of these insecticide from the beneficial effects of preventing ticks. Again, I tend to compromise and only use the topical during the greatest incidence of tick usually in the spring and fall. It is all a balance! Keep your pets away from tick infested areas, check them daily and stay healthy and happy and tick free!!